Centering Equity in the Digital Transformation of Primary Health Care
Findings from Digital Health Exemplars’ research on enablers for digital transformation in primary healthcare
Issue 21, April 2025
In this month’s edition of the Digital Health Research Roundup, Dr. Binyam Tilahun, Dr. Amare Tariku, Betelhem Abebe, and Lena Kan serve as our guest editors, offering reflections on digital health equity as both a core principle and a strategic enabler of digital transformation in health systems. Drawing from seminal literature and key findings from the Digital Health Exemplars (DHE) project, this issue explores how equity can be meaningfully embedded in the design, implementation, and scaling of digital health interventions—particularly within primary healthcare (PHC) systems. Dr. Tilahun and the DHE team highlight some of the key challenges–and strategic responses–countries at different levels of maturity have encountered in advancing equity-centered, digital health transformation.
Guest Editors’ Remarks:
The WHO Universal Health Coverage Declaration emphasizes health equity as a central goal in achieving universal health coverage. Health equity means that all individuals, regardless of socio-economic status, race, gender, or location, have a fair opportunity to achieve optimal health. However, significant disparities persist in health service access and delivery on a global level, with marginalized populations facing worse health outcomes due to limited access to healthcare services, especially in most of the low- and middle-income countries (LMICs).
The exponential growth in the health sector’s adoption of digital health technologies over the past decade has improved access to, and the quality of, health service delivery at PHC facilities, as well as the availability of essential drugs and supplies. Systematic reviews indicate that increased access to digital health technologies improves maternal, child, and other healthcare service coverage in primary healthcare.

Despite these gains, people of lower socioeconomic status, with less schooling, and in rural areas are disadvantaged in terms of access to digital health interventions. The recent COVID-19 pandemic also highlighted and worsened these disparities, making health equity more urgent than ever. These gaps underscore the critical importance of intensifying efforts to combat social, geographic, and other forms of inequities in digital health technologies. Without applying a deliberate equity lens to digital health design and implementation, we risk reinforcing long standing structural barriers, creating a digital divide in healthcare. Regularly identifying the patterns and attributes of this divide is essential for shaping national and global efforts aimed at improving equitable access to digital health interventions and, consequently, PHC services. A helpful guide for doing so is the recently published Digital Health Equity Framework which outlines practical ways to embed equity at every phase of a digital health journey, from planning to evaluation. (See CGDHI’s October 2024 Research Roundup which covered this valuable resource in detail.)
To understand how equity enables the successful digital transformation of PHC, the Digital Health Exemplar (DHE) project team investigated the experiences and outcomes in five DHE countries: Rwanda, Ghana, India, Brazil, and Finland. Using the Digital Health Equity Framework to guide their research approach, the team examined how equity was considered in the design, implementation, and impact of digital health programs and policies in each of the countries.
This month's Roundup shares some of the DHE project findings on digital equity, highlighting lessons learned on the challenges posed by the digital health divide and the strategies implemented within the DHE countries to address the observed inequities. We also feature foundational publications on digital equity, including the aforementioned Framework and Richardson et al.’s writing on the Digital Determinants of Health. Taken together, these resources demonstrate how digital health technologies, when implemented with an equity focus, enhance efficiency and equitable access to quality primary healthcare services.
Foundational Publications on Digital Health Equity
Evidence- and Consensus-Based Digital Healthcare Equity Framework
E. Hatef, M. Austin, Evidence- and Consensus-Based Digital Healthcare Equity Framework, Agency for Healthcare Research and Quality, 2024
The Digital Healthcare Equity Framework and its Implementation Guide are practical resources for ensuring that digital healthcare solutions are developed and applied in ways that reduce, and not exacerbate, healthcare disparities. While based on US-focused evidence, these resources offer foundational guidance and strategies that can be applicable to many types of settings, including countries at different stages of digital development.
See our October 2024 Research Roundup for a summary of these resources, including tips on adapting the foundational guidance and strategies to global contexts.
A Blueprint for Digital Health Equity
S. Richardson et al, A Framework for Digital Health Equity, NPJ Digital Medicine, 2022
This article proposes an expanded framework for digital health equity by introducing the concept of Digital Determinants of Health (DDoH) across individual, interpersonal, community, and societal levels. Emphasizing the importance of embedding equity into the digital transformation of healthcare, it provides a use case on remote patient monitoring (RPM) to illustrate the framework’s practical application.
Key Takeaways:
- The Digital Determinants of Health (DDoH), such as digital literacy, broadband access, implicit tech bias, and algorithmic bias, operate across individual, interpersonal, community, and societal levels. These determinants shape access to–and benefits from–digital health tools. Ignoring these determinants risks exacerbating existing health disparities.
- The framework calls for an “upstream,” multi-level approach to implement digital equity, stressing that most interventions overly target individual behaviors. They overlook critical systemic and structural barriers that more deeply affect marginalized populations, such as technology infrastructure and policy limitations.
A practical use case on RPM demonstrates how equity-focused design—including inclusive user interfaces and opt-out enrollment—can improve accessibility for underserved users. The approach also emphasizes the importance of community partnerships to support patient engagement and trust, as well as policy reforms that ensure reimbursement, data privacy, and sustainable scaling of digital health tools in marginalized settings.
Mapping Equity in Kenya’s Digital Health Ecosystem
Ruth Wambua et al, The Combined Effects of Digital Health Interventions on Universal Health Coverage Equity in Kenya: An Integrated Approach, Journal of Science, Innovation and Creativity, 2025
This study evaluates the collective impact of digital health tools, services, programmes, and information systems on equitable access to UHC in Kenya, with a focus on Makueni County. Using a quantitative survey of 348 participants and structural equation modeling, the authors demonstrate how integrated digital health interventions can influence various dimensions of UHC.
Key Takeaways:
- Integrated digital health interventions—including tools and technologies, services, programmes, and information systems—were strongly associated with improvements in equitable access to UHC. A robust structural equation model showed that, together, these components explained 96.6% of the variance in access outcomes. Among them, digital health programmes and services emerged as the most influential, highlighting their critical role in driving health equity in resource-limited settings.
- Digital literacy, infrastructure gaps, and socio-economic inequalities remain critical barriers, especially for older adults and rural residents. Despite 63.8% smartphone ownership, limited awareness and engagement with advanced digital tools constrained the impact of digital health interventions.
Policy-level support for advancing digital health equity exists but suffers from implementation challenges. Infrastructural deficits such as poor internet and electricity access, and regional disparities in digital adoption, undermine efforts to ensure inclusive and equitable access to care under Kenya’s national eHealth strategy.
Key Insights from the Digital Health Exemplars Project
As part of the Digital Health Exemplars project, CGDHI and its partners explored the challenges and gaps in digital health equity, focusing on strategies to promote inclusive and equitable design, development, and access to digital health interventions. Through interviews with key stakeholders in each country, we gained valuable insights into effective approaches for bridging the digital divide in health system transformation. Below is a summary of our key findings on advancing digital health equity.
Overall Strategy Recommendations:
Expand mobile health access and prioritize user-centered design
Design digital health solutions with cultural and linguistic adaptability to create meaningful access and use of these solutions, ensuring true digital inclusion, especially for marginalized communities.
Dedicate strategies to promote gender equity in digital health
Ensure gender representation in the digital health workforce—particularly in leadership and decision-making roles, such as mandating gender quotas, investing in education and mentorship, and fostering inclusive, flexible work environments.
Target digital health financing in more rural areas
Invest in rural infrastructure and implement targeted, equity-based financing models that prioritize hard-to-reach areas and respond to specific regional digital needs, to ensure that digital health reaches everyone, no matter where they live.
Implement inclusive and targeted digital literacy programs
Promote tailored digital mentorship and support networks as well as context-specific training initiatives to address the diverse needs of health workers, particularly those facing additional vulnerabilities such as age or disability.
Equity Challenges Encountered in DHE Countries and Strategies Used in Response:
Challenge #1:
Marginalized and vulnerable groups, including ethnic and minority groups, as well as communities from lower education and wealth groups, are at risk of digital exclusion due to various language, cultural, and physical barriers. To achieve true digital inclusion in health, digital health interventions must be thoughtfully designed with a user-centered and inclusive approach from the outset. Equally important are scaling strategies that account for the diverse cultural, social, and contextual realities of different communities to ensure their equitable access to, meaningful use of, and benefit from digital health solutions.
Strategies Used by DHE Countries to Address Digital Exclusion:
Finland: Nationwide prioritization of equity
In Finland, digital inclusion is a national priority. Academic institutions, government bodies, and public organizations have launched several initiatives and research efforts to ensure that socially vulnerable groups—including people with disabilities, those with mental health challenges, immigrants, and prison populations—can access and benefit from digital health services.
Rwanda: Multiple language options in digital services for health
In Rwanda, there are targeted mechanisms to narrow the language barriers in using digital health solutions. Rwanda’s Kwivuza platform—an electronic medical insurance service—addresses language barriers by offering multiple language options, making it more accessible to a broader range of users.
Ghana and Rwanda: Improvements to mobile phone access
The rise in mobile phone ownership offers a unique opportunity to engage broader populations and improve health outcomes. In countries such as Ghana and Rwanda, greater access to mobile phones has been significantly linked to earlier initiation of antenatal care (ANC), higher rates of full immunization, and increased use of modern contraceptives. While both countries have made progress in reducing disparities in mobile phone ownership based on wealth and education (Figure 1 & 2), gender-based gaps persist. Addressing these gender inequities—particularly by expanding women’s access to mobile phones—could play a critical role in enhancing women’s ability to access and utilize quality health services.
Findings on Inequities in Mobile Phone Ownership in Ghana and Rwanda
The graphs below highlight persistent wealth- and education-based inequities in mobile phone ownership across both Rwanda (2010–2020) and Ghana (2008–2022). Ownership remains significantly lower among the poorest households and those with no formal education, despite national-level gains. Notably, women across both countries consistently report lower ownership than household averages, with equity gaps by wealth and education especially pronounced in more recent years.
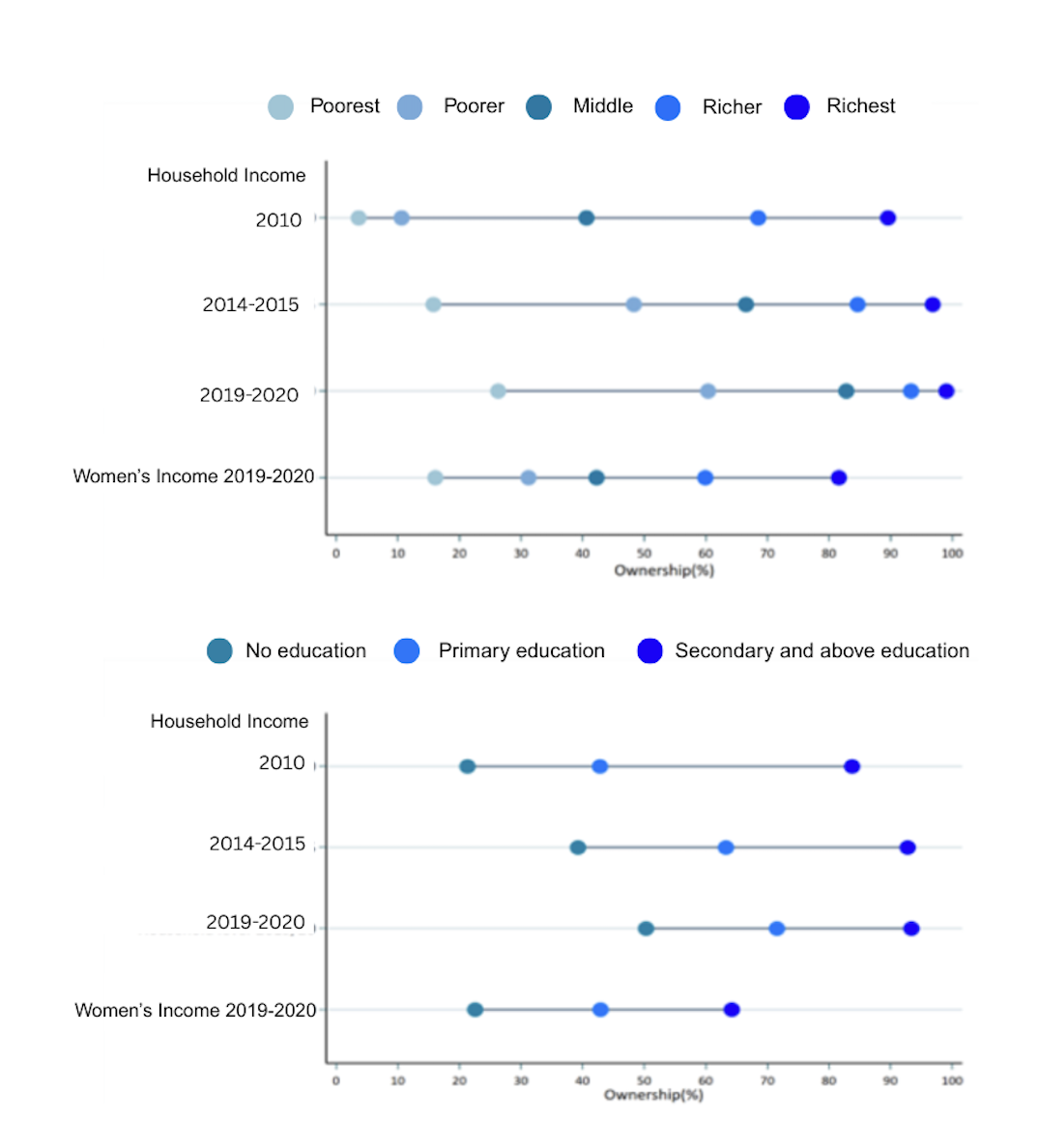
Figure 1: Equiplots illustrating wealth (A) and education (B) based inequities in mobile phone ownership in Rwanda, 2010 -2019/20.
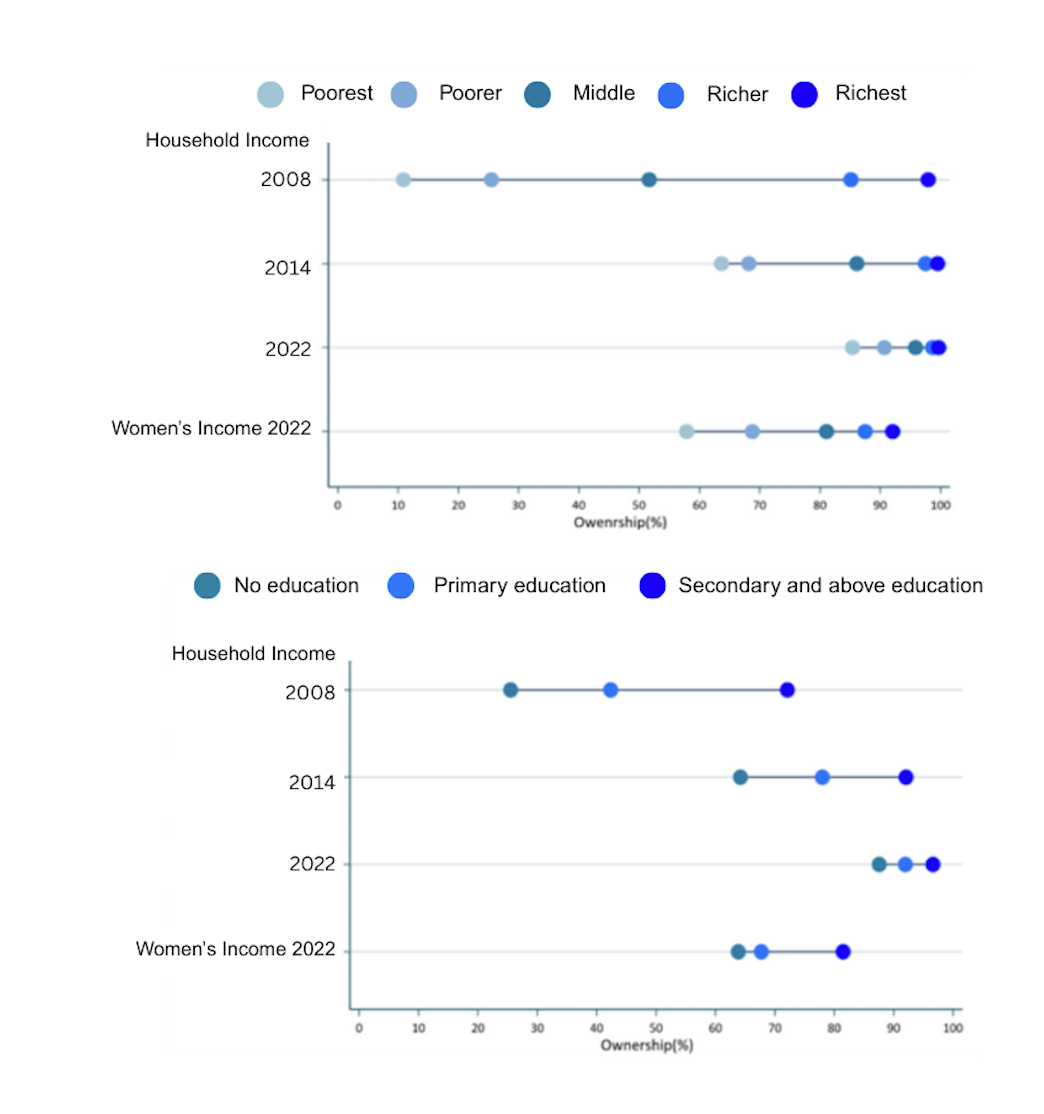
Figure 2: Equiplots illustrating wealth (A) and education (B) based inequities in mobile phone ownership in Ghana, 2008-2022.
Challenge #2:
Gender representation in the health ICT workforce and at the overall digital health decision-making level remains unequal, particularly in countries with emerging digital health systems. Despite women making up a significant portion of the overall health workforce, they are often underrepresented in leadership and decision-making roles within digital health. This imbalance reinforces existing gender power disparities and limits the inclusivity of digital health transformation.
Strategies Used by DHE Countries to Address Gender Inequity in the Digital Health Workforce:
Finland: Policies promoting women in digital health governance roles
In Finland, gender quotas at the organizational level mandate equal representation of women in leadership and decision-making roles. This contributes to more balanced gender representation in digital health governance. However, representation of immigrant populations in these spaces remains limited and is an area requiring greater focus and inclusion.
Ghana: Capacity-building for young women in the digital health sector
In Ghana, gender equity in the ICT sector is being advanced through initiatives such as the Girls-in-ICT program. This initiative provides training and opportunities for young women at the subnational level to build skills and pursue careers in the technology and digital health sectors.
Challenge #3:
Significant regional and geographic disparities persist in access and use of digital health interventions—particularly in rural, remote, and hard-to-reach areas with limited digital infrastructure. These gaps highlight the urgent need for targeted, context-specific strategies to ensure that comprehensive digital health services are equitably extended beyond urban centers. Addressing the urban-rural divide is essential for achieving geographic equity in digital health access and utilization.
Strategies Used by DHE Countries to Address Geographic Inequity of Digitization:
Brazil: Equity-based financing mechanisms
Equity-based financing mechanisms in Brazil direct federal financing to municipalities based on their health digitalization needs. Informatiza APS helped improve computerization of health facilities. More recently, the SUS Digital Program allocates financing to states and municipalities based on a digital maturity index (ICSD) which takes into account rurality, social vulnerability, connectivity, and workforce distribution.
Ghana: Targeted financing for rural telecommunications infrastructure
The Ghana Investment Fund for Electronic Communications (GIFEC) leads the Ghana Rural Telephony and Digital Inclusion project. This project aims to enhance connectivity in underserved rural areas. The initiative is supported through various funding sources, including corporate social responsibility contributions from major telecommunications companies, to strengthen rural digital infrastructure and promote inclusive access.
Challenge #4:
Frontline health workers display varying levels of digital literacy and capacity, with those in remote areas or from lower socioeconomic backgrounds often facing greater difficulties in effectively using digital health tools. These challenges are further intensified by intersecting vulnerabilities—such as older age, disabilities, mental health conditions, and limited access to training—especially among female health workers. Bridging these gaps through inclusive capacity-building and targeted support is essential to ensure equitable participation in the digital health workforce.
Strategies Used by DHE Countries to Address Health Workers’ Digital Literacy:
Finland: Digital literacy promoted at national and subnational levels
In Finland, the Ministry of Education and Culture plays a central role in promoting digital literacy nationwide. At the subnational level, decision-makers are responsible for organizing digital support networks to meet local needs. One key initiative, MEDigi, provides a unified platform for training, teaching, and assessing the digital competencies of health professionals, ensuring they are equipped to navigate an increasingly digital healthcare environment.
Finland: Research on inequities of burden of digital health technologies on health workers
Finland is conducting research to address the disproportionate job strain experienced by female health workers compared to their male colleagues. These efforts include examining the stress linked to the use of digital systems in healthcare, with a focus on reducing the burden caused by managing multiple, often fragmented, digital platforms. The goal is to develop more sustainable, user-friendly solutions that better support healthcare providers in their daily work.
Rwanda: Mentoring for health workers on digital health
In Rwanda, a mentorship program has been established to improve health worker’s competency with digital tools. This program provides much-needed support to health providers with limited digital skills when using Epi-Tracker, the national electronic immunization registry.
Click the links below to read previous editions of Research Roundup, to learn more about our DHE Project findings, and to receive the latest updates in global digital health!
Meet Our Guest Editors:

Dr. Binyam Tilahun (PhD) is Professor of Digital Health and Implementation Sciences at the University of Gondar, Ethiopia where he is a founder and Director of the Center for Digital Health and Implementation Sciences. With more than 15 years of global research experience in digital health, data science, and implementation sciences he has recently led numerous externally funded projects, working closely with WHO, UNICEF, Africa CDC, Gates Foundation, and Doris Duke Charitable Foundation among others. He is currently working as an advisor to the Ethiopian Ministry of Health in the Health Information Systems Technical Working Group.
Betelhem Abebe (MPH) is a Researcher at the Center for Digital Health and Implementation Sciences (CDHI), University of Gondar, Ethiopia. She holds a Master’s degree in public health with a specialization in epidemiology from the University of Gondar. Betelhem has experience in epidemiological research and statistical analysis, and also has led qualitative and quantitative research. Through her research on maternal and child health, she has authored numerous peer-reviewed publications. Betelhem continues to contribute to advancing public health through implementation science and digital health innovations.
Dr. Amare Tariku (PhD) is Associate Professor of Nutrition and Public Health at the University of Gondar, and an implementation research scientist at the Center for Digital Health and Implementation Sciences (CDHi), University of Gondar, Ethiopia. He has led projects on maternal and child health, nutrition, health systems, digital health, and implementation science research, funded by the Bill and Melinda Gates Foundation, Fogarty International Center at the NIH, Research for Health in Humanitarian Crises, etc. He is currently providing technical support to the Ethiopian Ministry of Health.
Lena Kan is a Researcher with the Johns Hopkins Center for Global Digital Health Innovation. Her interest primarily lies in the intersection of digital health and PHC, and the use of data to generate evidence for decision-making. She has published several academic papers and reports on various topics, including health systems transformation, community-based health information systems, maternal mortality estimation, and digital health. She holds an MSPH from Johns Hopkins Bloomberg School of Public Health.
